
Twin studies have also found a low concordance rate between monozygotic twins, with a 25% concordant for type 1 narcolepsy and 32% when looking at both type 1 and type 2 narcolepsy (Mignot, Citation1998). A family history of narcolepsy is uncommon however, family members are at an increased risk of 1–2% for first degree relatives (Billiard et al., Citation1994 Mathew, Citation1994). Often, if age of onset is in the teenage years there is a higher frequency of cataplexy experienced by the diagnosed individual (Krishnamurthy, Nallamothu, & Singareddy, Citation2014). Narcolepsy can develop at any age however, research has identified bimodal peak ages of onset of 14.7 and 35 years, with an average age of 16 (Silber, Krahn, & Slocumb, Citation2005).
It is now estimated that the prevalence for narcolepsy with cataplexy is between 25 to 50 per 100,000 (Longstreth, Koepsell, Ton, Hendrickson, & van Belle, Citation2007 Nohynek et al., Citation2012 Partinen et al., Citation2012) and 20 to 34 per 100,000 for narcolepsy without cataplexy (Shin et al., Citation2008 Silber et al., Citation2002). Some researchers have attempted to identify the prevalence rate of narcolepsy with and without cataplexy separately. These prevalence rates reflect both narcolepsy with and without cataplexy. However, other studies have estimated a much lower prevalence rate of 15 per 100,000 people (Shin et al., Citation2008).

American studies have estimated a higher prevalence of 56 per 100,000 (Silber, Krahn, Olson, & Pankratz, Citation2002).
Narcolepsy is a disabling sleep disorder with an estimated mean prevalence of approximately 30 per 100,000 people (Abde-Khalek, Citation2001 Cave, Citation1931 Daniels, Citation1934 Martikainen, Hasan, Urponen, Vuori, & Partinen, Citation1992 Ozdemir et al., Citation2005 Partinen & Hublin, Citation2005 Schmitt, Gugger, Augustiny, Bassetti, & Radanov, Citation2000 Schwegler et al., Citation2006 Szklo-Coxe, Young, & Mignot, Citation2003 The Gallup Organization, Citation1997 Young et al., Citation1993). A greater understanding of the role of hypocretin in these health complaints could aid in the development of more appropriate treatments for pain, migraines and headaches amongst people with and without narcolepsy. This review poses a number of research questions that need to be explored about whether the presence or absence of cataplexy is differentially associated with different types, severity and location of chronic pain frequency, location and types of migraines and headaches and general health and wellbeing among people with narcolepsy. Also, it is unclear whether general health and wellbeing (including psychological wellbeing) is similarly affected by hypocretin levels, or may be confounded by different levels of other health symptoms, such as pain. Currently, there are no studies published to determine whether pain, migraines and headaches are just common symptoms experienced by all people with narcolepsy or whether the presence of the cataplexy symptom (and thus assumed low levels of hypocretin) exacerbates these symptoms. However, these studies have not compared findings across narcolepsy with and without cataplexy.
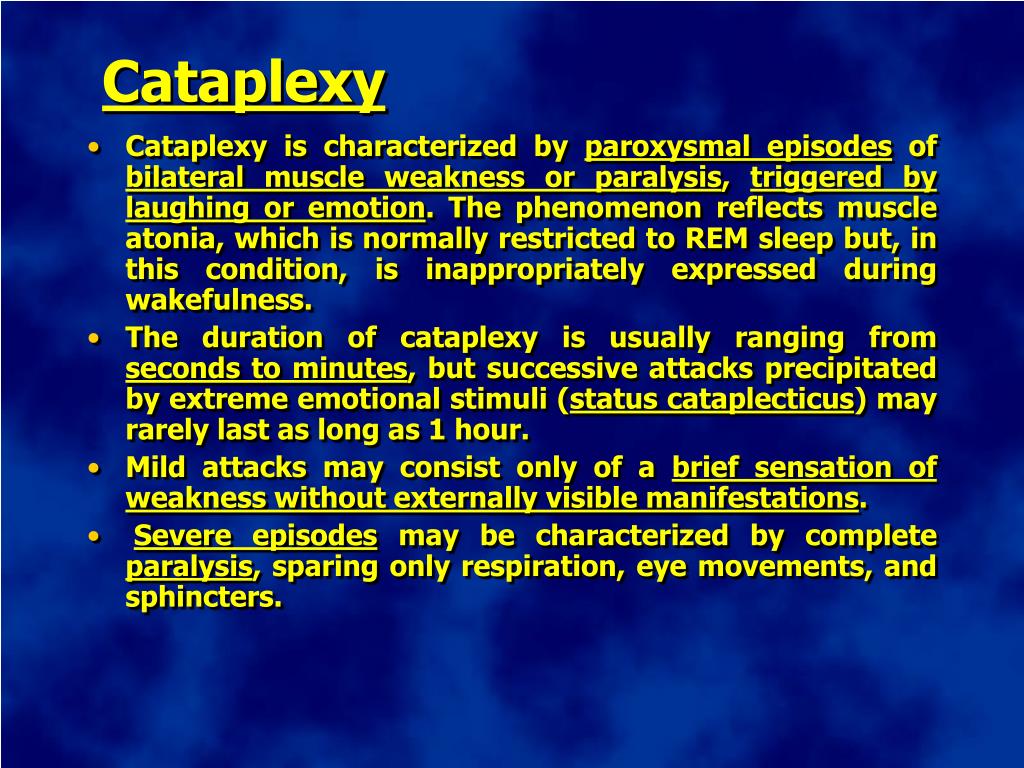
There is evidence to suggest that hypocretin may have an association with pain, migraines and headaches in people with narcolepsy. The presence of cataplexy in people with narcolepsy has a well-documented tight association with very low or non-detectable levels of the central nervous system neuropeptide, hypocretin (also termed orexin) while levels of hypocretin are normal in people with narcolepsy without cataplexy.


 0 kommentar(er)
0 kommentar(er)
